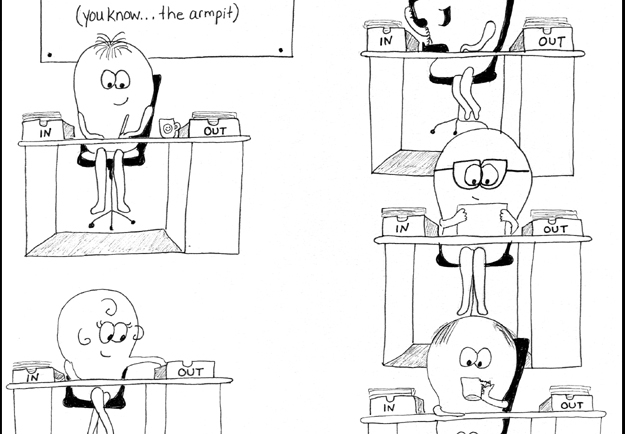
Self-Manual Lymphatic Drainage – Arm/Upper Extremity
This video is intended to show you how to perform self-manual lymphatic drainage (or “self-MLD”) for an upper extremity. If you have swelling in your arm, hand, or upper trunk, these strokes, performed in this demonstrated...