How Does Lipedema Become a Fluid Problem?
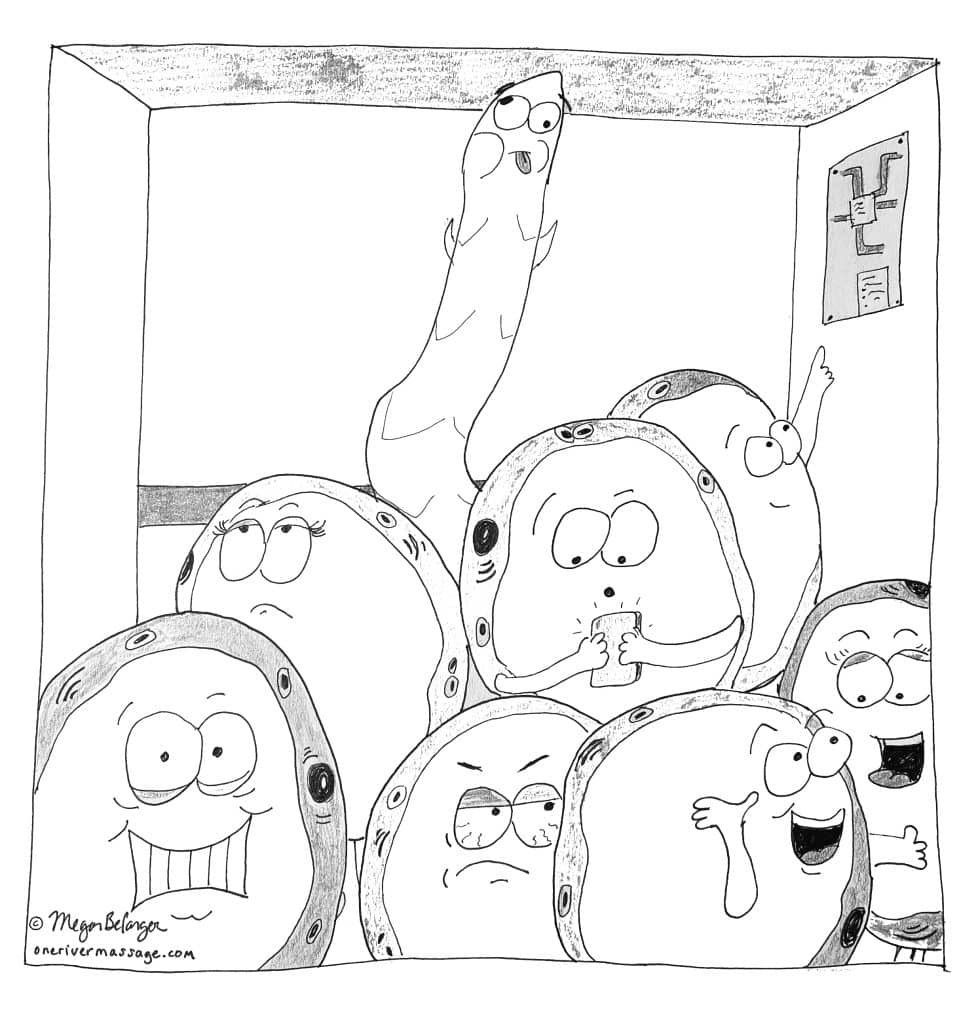
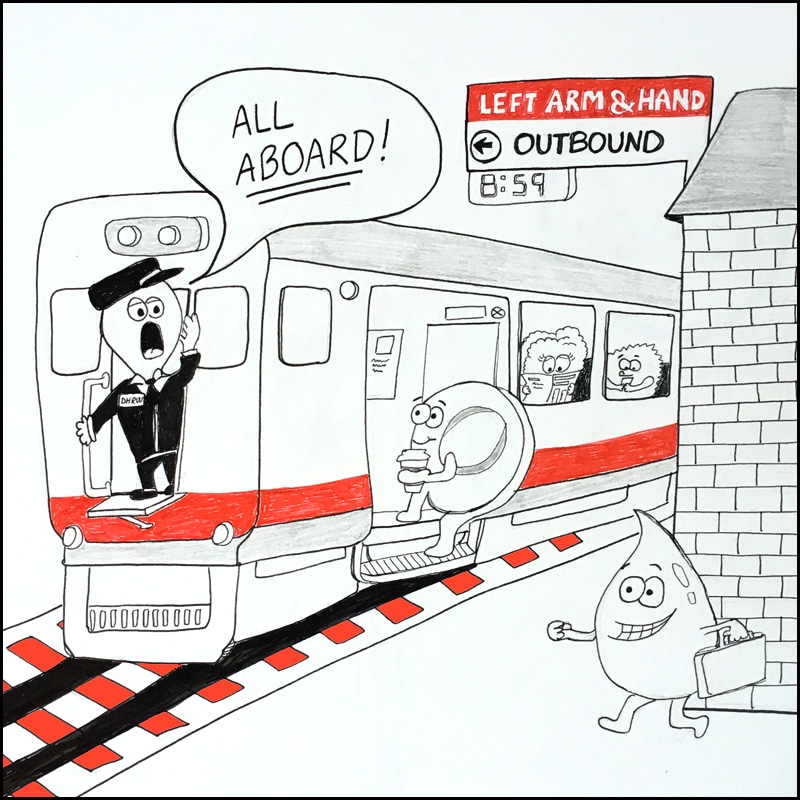
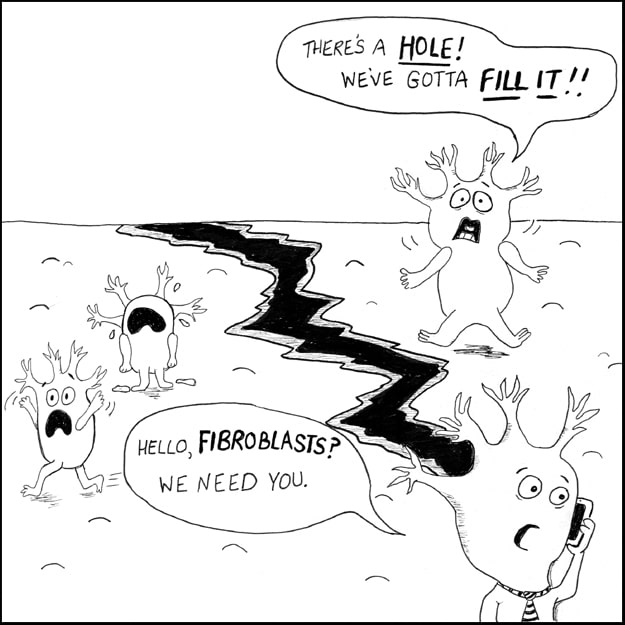
We know that the disease lipedema involves an impairment of fat cell distribution and deposition (hyperplasia or hyperproliferation) and that this usually occurs symmetrically in the body, so in both legs (and sometimes both arms). You might hear about fat cells being called by their clinical name, adipocytes. But how does lipedema become a fluid […]
How Does Lipedema Become a Fluid Problem? Read More »